
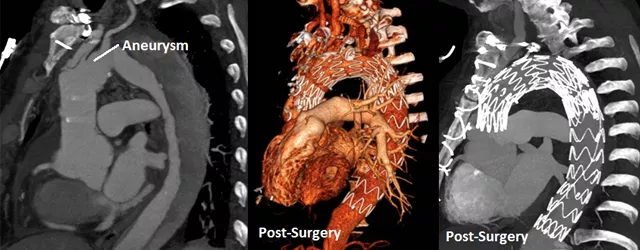
Andy Alvarez, 67, lost his voice—and almost his life—following surgery for a thoracic aortic dissection/aneurysm. An aneurysm is a “ballooning” in the chest cavity of a weakened aorta, the artery that carries blood from the heart to the rest of the body. Today, as Alvarez is celebrating his latest test results, he is speaking out to advise others about how to beat this “silent killer.”
In October 2015, Alvarez had chest pain when he when he was rushed via ambulance from his home in Lowell to a local ER. Though he was once a smoker and was on medication for blood pressure and cholesterol, he had no family history of aortic disease and previously didn’t have any symptoms, which is typical with this condition. He also didn’t have the opportunity to discuss his medical treatment plan at that point because he fell into a coma when he was helicoptered to Tufts Medical Center for emergency surgery.
“I didn’t realize what was happening until I came out of surgery,” says Alvarez. “I saw my surgeon and said, ‘I guess you saved my life.’”
A rare but dangerous condition
Thoracic aortic aneurysms, while not as common as abdominal aortic aneurysms, affect approximately 15 per 100,000 Americans every year. Of that number, about one-third has a dissection, a tear that occurs between the layers of the aorta, forcing the layers apart.

“Thoracic aneurysms/dissections are very dangerous conditions that require very specialized treatment,” says Payam Salehi, MD, PhD, Alvarez’s vascular surgeon at Tufts MC. “A challenge with dissections and aneurysms is that they are hard to detect without the benefit of diagnostic testing such as CT scans, MRIs and ultrasounds. Some people aren’t even aware they have a thoracic aneurysm, and not all of those diagnosed with this condition need immediate surgery, but we strive to prevent ruptures, because those are life-threatening.
“Andy’s case was extremely complicated, but he has survived.”
Weathering the first several surgeries
Treatment options for this condition include monitoring, minimally invasive surgery, traditional open surgery and hybrid procedures. In Alvarez’s case, the initial treatment was clear: Alvarez’s cardiac surgeon and Dr. Salehi performed open chest surgery, which involved removing the damaged section of the aorta and replacing it with a synthetic tube, or graft. While the procedure went well, Alvarez suffered a stroke after being admitted, and two weeks later, a second bypass surgery lasting 20 hours was required to repair a descending dissection of the artery.
Compounding the second surgery, Tufts MC’s medical team determined that Alvarez also needed thoracic endovascular aortic repair (TEVR), a minimally invasive procedure in which a catheter is used to insert a thin tube called a stent graft that reinforces the aneurysm and helps prevent it from bursting. A month of hospitalization was followed by two weeks of rehabilitation, and Alvarez returned home, hopeful that he would recover without further intervention but mindful that he needed to maintain a healthy lifestyle and check for aneurysm growth.
Six months later, in April 2016, after a couple of checkups, Alvarez suffered another setback due to an endovascular leak and dissection. This necessitated another bypass operation with Dr. Salehi. The successful procedure was followed by the familiar drill of hospitalization and rehabilitation.
Finally, in November 2017, Alvarez required a second TEVR by Dr. Salehi to treat an abdominal aortic dissection. Unlike open surgery, this procedure results in less bleeding and faster recovery.
The voice
Alvarez was also dealing with an additional complication, however—hoarseness as a result of damage to his right vagus nerve during his first operation—and he was losing his voice. To restore his vocalization, he received injections in his vocal chords and then tracheoplasty surgery to open his airways.
“One-third of patients don’t survive open aneurysm surgery in the acute setting,” says Dr. Salehi. “Every patient is unique, and personalized care from medical specialists is critical. Fortunately, we at Tufts have been involved in promising clinical trials and have benefited from major advancements in technology. A few years ago, patients like Andy probably wouldn’t have made it.”
Alvarez is optimistic following his most recent tests at Tufts MC that showed no further issues. And his voice is animated when he talks about his medical experience: “I’m happy to speak up and encourage other patients to seek the best medical treatment,” he says. “I look forward to my walks and my visits to the senior center. I’m happy to be alive.”

