What is congestive heart failure?
In CHF, your heart muscle becomes stiff or weak, making it hard for your heart to pump enough blood to your organs and tissues. When this happens, blood and fluid get backed up and can become “congested” in your lungs, legs, feet, arms and other organs.
Who is at risk for congestive heart failure?
As we age, the risk for CHF increases, even in healthy adults. People who are 65 and older have a higher risk of heart failure, as do people with a family health history, high blood pressure, diabetes, obesity, smoking and an inactive lifestyle.
Anyone can develop CHF, but certain racial groups are disproportionately affected. CHF rates are higher in Black populations than for other races and ethnicities. Black people also have the highest death rates from heart disease when compared to other groups. If you’re in a higher risk group, it’s important to visit your doctor for regular blood pressure and heart rate checks.
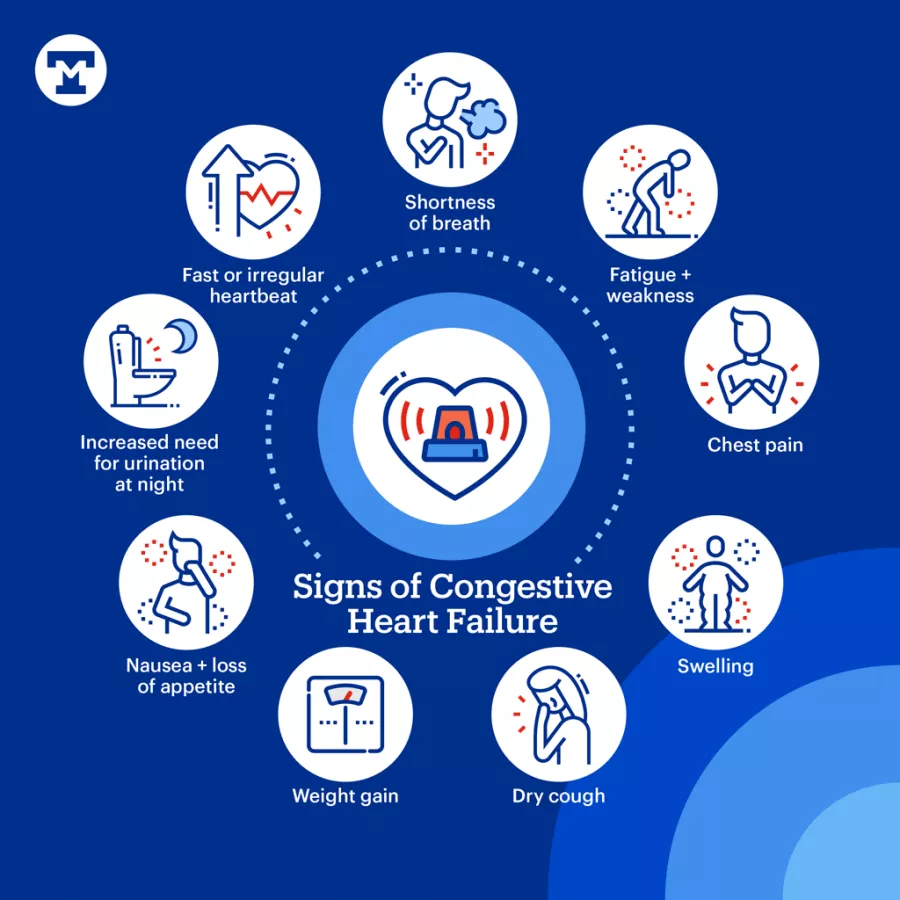
Signs of congestive heart failure
Symptoms and signs of CHF can be easy to miss, especially since they can mimic other medical conditions. You should talk to your doctor if you have any of the symptoms below. The earlier you get treated, the better your chances of controlling your symptoms.
Shortness of breath
CHF causes fluid buildup in the lungs, making breathing harder and causing shortness of breath during physical activity and after sitting or lying down. If you notice you are winded doing regular activities or sleeping, it could be a warning sign of CHF.
Fatigue and weakness
People with CHF feel tired and weak because their hearts aren’t able to pump the amount of blood their body needs to function well. CHF can result in people feeling constantly exhausted, weak and lightheaded.
Chest pain
Chest pain is an early symptom of CHF. There are several types of chest pain, and it’s important to know the difference. Pressure or tightness in the chest is called angina, usually lasting only a few minutes. Chest pain that happens suddenly and with other symptoms, such as sweating and nausea, can be a more serious sign of a heart attack.
Swelling
CHF can cause fluid to build up in your feet, ankles, arms and legs. Retaining too much fluid will cause swelling or edema and can indicate worsening heart failure.
Dry cough
Fluid accumulating in the lungs can cause chronic coughing or wheezing. The dry, hacking cough may worsen at night or when lying down.
Weight gain
Rapid weight gain can be a sign of fluid retention and worsening heart failure. Be on the lookout for sudden changes in your weight or unexplained weight gain.
Nausea and loss of appetite
CHF can cause a loss of appetite and nausea. It can also cause fluid to back up in your stomach, making you feel bloated or full even after eating a small meal.
Increased need for urination at night
During the day, your heart has difficulty moving blood through your body, including your kidneys, which produce urine. At night, when you’re lying down, your kidneys can easily filter water from your blood. Peeing too much at night, or “nocturia,” can disrupt your sleep quality, making you tired during the day.
Fast or irregular heartbeat
If you have CHF, your heart works overtime to send blood throughout your body. When your heart beats faster, it can feel like heart palpitations or a fluttering in the chest.
Types of congestive heart failure
CHF can happen on the left side, right side or both. Each type of failure has specific symptoms.
Left-sided heart failure
Left-sided heart failure occurs when the left ventricle loses its ability to contract (systolic failure) or relax (diastolic failure), causing the left side to work harder. Signs of left-sided heart failure are shortness of breath, swelling/fluid retention, weight gain and coughing.
Right-sided heart failure
Right-sided heart failure occurs when the right side is unable to pump blood to the lungs, causing swelling and shortness of breath.
Biventricular heart failure
Biventricular heart failure is when both sides of the heart are affected, causing a combination of left and right-sided heart failure symptoms.
What are the stages of congestive heart failure?
Heart failure is a chronic disease that gets worse over time. There are 4 stages of heart failure, from early to advanced.
Stage A
Stage A, also known as pre-heart failure, means you are at high risk of developing heart failure because you have a family history or medical conditions linked with heart failure, such as high blood pressure, diabetes, coronary artery disease, alcohol misuse and metabolic syndrome.
There are no symptoms at this stage of heart failure. People with a high risk of developing heart failure should manage their risk by making healthy lifestyle choices such as exercising every day.
Stage B
This stage of heart failure occurs when there are signs that your heart isn’t pumping well. You may not show any symptoms of CHF at this stage. Your doctor may recommend medication.
Stage C
Stage C heart failure begins at the first sign of CHF symptoms. At this stage of heart failure, you likely are tired, are short of breath during normal activities and have trouble exercising. Your doctor will recommend medications to strengthen your heart muscle and improve symptoms
Stage D
This stage is the most advanced stage of heart failure when symptoms generally don’t improve with treatment. Your doctor may suggest heart surgery, a heart transplant or ventricular assist device.
Diagnosing and treating congestive heart failure
Detecting CHF early is crucial to managing symptoms and getting timely treatment. Common tests used to diagnose CHF include blood tests that measure proteins that increase in CHF, electrocardiogram (EKG) to measure your heartbeat and echocardiogram to look at the size of your heart and how well it's working.
Once your doctor diagnoses your CHF stage, they will recommend medication, lifestyle changes and surgical options like pacemakers, heart transplant or left ventricular assist device. CHF is a chronic disease that requires ongoing care and monitoring to manage symptoms and prevent complications.

Preventing congestive heart failure
You can prevent CHF by paying close attention to your heart health. Eating heart-healthy foods that improve blood flow, exercising regularly, avoiding excessive drinking and not smoking will go a long way to keeping your heart strong.
Maintain a balanced diet
Eat a colorful diet rich in fruits, vegetables, whole grains and proteins. Reduce or avoid salty, sugary foods and unhealthy fats that can lead to high blood pressure and cholesterol.
Regular exercise
One of the best things you can do for your heart is to move your body daily by walking, jogging or swimming. Exercising strengthens your heart muscles and improves your overall cardiovascular health.
Manage blood pressure
Managing your blood pressure keeps your heart muscle strong and working properly. You should monitor your blood pressure and talk to your doctor about ways to manage high blood pressure.
Monitor blood sugar levels
People with diabetes are at risk for developing heart disease. Keeping blood “sugar” or glucose levels low will keep blood vessels from being damaged. Track your blood sugar levels and get screened regularly.
Quit smoking
Quit smoking. Smoking damages your heart, reduces the flow of blood and increases your risk of developing plaque buildup, called atherosclerosis, which can lead to a heart attack. Even if you’re not a smoker, secondhand smoke is bad for your heart. Your doctor can talk to you about ways to quit and connect you with programs and resources.
Limit caffeine
Too much caffeine can worsen heart failure. To avoid overstimulating your heart, you should have no more than 2 servings of caffeine daily. Replace caffeinated drinks with water, herbal tea or decaffeinated options.
Get regular heart health screenings
Make regular health screenings a priority. Monitoring your heart health can lead to early detection. If you have concerns about your heart health, check-ups are your chance to be proactive and talk to your doctor.
Take charge of your heart health
We're dedicated to providing exceptional care for those affected by congestive heart failure. Our expert team utilizes advanced diagnostic tools and personalized treatment plans to address your unique needs. We focus on not only managing symptoms but also on improving your overall heart health.
If you’re experiencing symptoms or are at risk for CHF, don't wait—take the first step toward a healthier heart today.
Let’s get your heart in shape. Schedule an appointment and learn more about cardiovascular care resources, support groups and clinical trial.


